Hormonal headaches: Understanding the connection between hormones and migraines in women
The Link Between Hormones and Migraines: A Guide for Women
Do you ever find yourself feeling irritable, nauseous, or completely debilitated due to a pounding headache that just won't quit?
If you're a woman, the culprit behind this all-too-common experience could be hormonal headaches, specifically linked to changes in oestrogen levels, which typically occur during your menstrual cycle, pregnancy, or menopause. Managing these progesterone headaches is crucial for reclaiming a sense of normalcy.
But don't worry; you're not alone. There are ways to effectively manage the symptoms and get back to feeling like yourself. In this blog, we'll delve into the science behind hormonal headaches, with a focus on progesterone headaches, and explore practical tips and treatments that can help you take control of your health and reduce the impact on your daily life. Whether you're a chronic sufferer or just looking to better understand your body, we've got you covered. Let's dive in!
Hormonal Headaches in Women: Understanding the Link to Migraines
Hormonal headaches, a common issue mainly affecting women, are closely linked to changes in two key hormones: oestrogen and progesterone. These headaches often cause severe migraines, with symptoms like nausea, dizziness, and sensitivity to light and sound.

Oestrogen, an important hormone in the menstrual cycle, plays a big part in these headaches. Many women get migraines when their oestrogen levels change, especially during ovulation, periods, pregnancy, and menopause. As oestrogen levels go up before a period and then suddenly drop, it can trigger bad migraines that last for days. Experts think these changes affect how the brain feels pain.
But it's not just oestrogen that's involved. Progesterone, another hormone in the menstrual cycle and pregnancy, can also cause headaches. Changes in progesterone levels, like from hormone treatment or certain contraceptives, might give some people headaches too.
Dealing with hormonal migraines can be tricky, but there are things you can try. Keeping track of your headaches to spot any triggers, finding ways to relax and exercise to reduce stress, making sure you get enough sleep, and thinking about hormone treatments like birth control pills or hormone replacement therapy can all help. Understanding how hormones affect migraines can help women better manage their headaches and maybe even have them less often or not as bad.
Preventing Hormonal Imbalance Migraines: Addressing Underlying Issues
Numerous women suffer from the interrelated issues of both hormonal imbalances and migraines. Hormonal imbalances can be a cause of headaches, but they can also exacerbate or worsen headaches that are caused by other factors. Therefore, addressing underlying hormonal problems is crucial to preventing headaches and promoting general health.
Numerous factors, such as stress, inadequate nutrition, and underlying medical conditions, can result in hormonal imbalances. Nevertheless, alterations in oestrogen levels are the most frequent cause of hormonal imbalances in women.
The hormone oestrogen regulates a woman's menstrual period, pregnancy, and other reproductive functions.
Hormonal imbalances can be brought on by changes in oestrogen levels, such as those that take place during adolescence, pregnancy, or menopause. In addition, hormonal imbalances that cause migraines can occur in women who use hormonal contraceptives or receive hormone replacement therapy.
Some of the more common causes of hormone imbalances include:
- Gut health: An imbalance in gut bacteria or intestinal permeability can lead to inflammation, which can disrupt hormone production and balance.
- Chronic inflammation: Inflammation throughout the body can disrupt the production and balance of hormones.
- Chronic stress: Chronic stress can cause an increase in cortisol levels and disrupt the balance of other hormones in the body.
- Nutrient deficiencies: A lack of essential nutrients, such as vitamins and minerals, can disrupt hormone production and balance.
- Toxins: Exposure to toxins in the environment, such as heavy metals and pesticides, can disrupt hormone production and balance.
- Medications: Hormone therapy, particularly high-dose oral contraceptives, can lead to initially high estrogen levels. It may take some time to adjust the dosage to achieve the right balance.
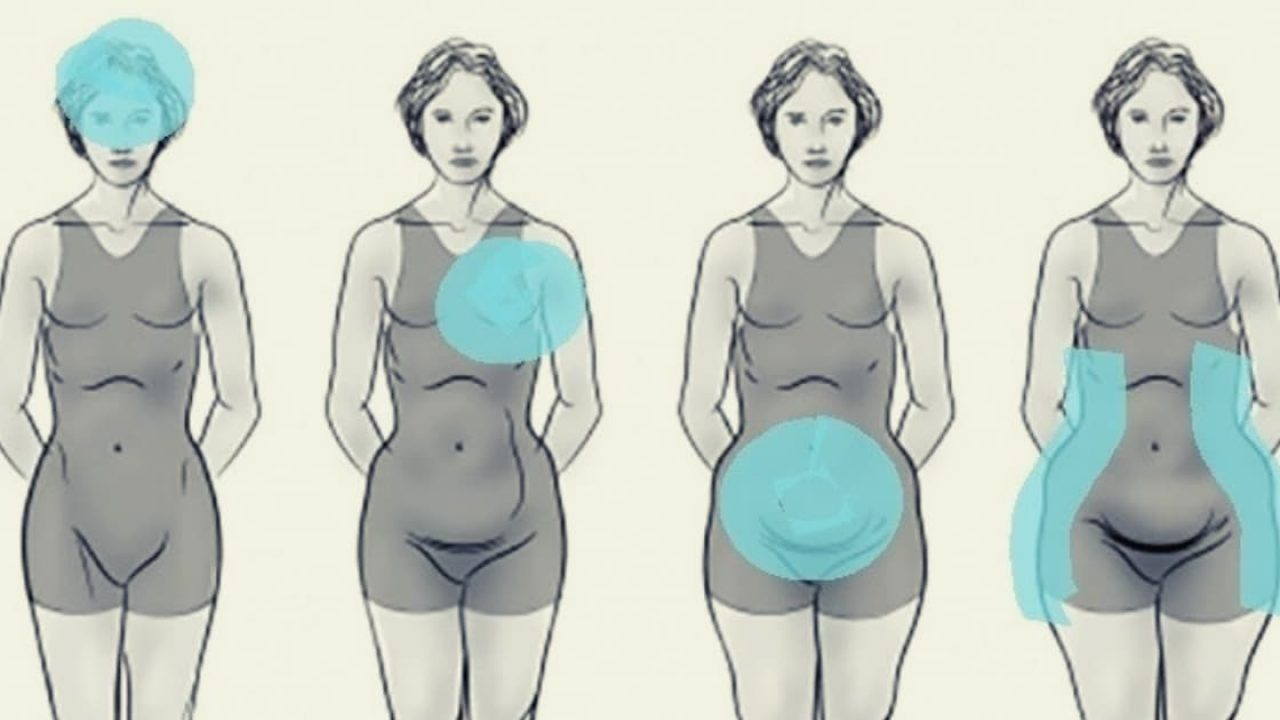
- Body fat: Adipose tissue or fat tissue secretes estrogen. Therefore, having a high percentage of body fat can result in high levels of estrogen.
- Stress: Stress triggers the production of cortisol hormone, which can deplete the body's ability to produce progesterone. This leaves estrogen unchecked in the body.
- Alcohol: Drinking too much alcohol can raise estrogen levels and hinder the body's ability to break down and metabolize estrogen.
- Liver problems: The liver plays a crucial role in breaking down and eliminating estrogen from the body. If the liver is not functioning properly, excess estrogen can accumulate. Digestive enzyme deficiency, dysbiosis, low magnesium levels, and insufficient fiber in the diet can all hinder the liver's ability to remove excess estrogen.
- Synthetic xenoestrogens: Synthetic xenoestrogens are chemicals found in the environment that mimic estrogen once inside the body. These chemicals, such as bisphenol A (BPA) and phthalates, can increase estrogen levels. Xenoestrogens are present in various plastics, pesticides, household cleaning products, soaps, and shampoos.
There are several environmental and lifestyle factors that can cause hormone imbalances, many of which people may not be aware of. However, this also presents an opportunity to effectively balance hormones using natural methods. By addressing factors such as medication use, body fat percentage, stress levels, alcohol consumption, liver health, and exposure to synthetic xenoestrogens, individuals can take steps to balance their hormones naturally. This can lead to improved overall health and well-being. It is important to work with a healthcare provider to identify the root causes of hormone imbalances and develop an individualized treatment plan.
Women's migraines must be prevented by addressing underlying hormonal issues. The following measures can be adopted to reduce the risk of hormonal imbalances and migraines:
- Maintain a wholesome diet: A nutritious and well-balanced diet can help regulate hormone levels and reduce the risk of migraines. Women should consume leafy greens, nuts, whole cereals, and fruits, which are rich in vitamins, minerals, and antioxidants.
- Tension management: Chronic tension can cause hormonal imbalances and migraines. Women should exercise relaxation techniques like yoga, meditation, and deep breathing to manage stress.
- Exercise regularly: Regular exercise can assist in regulating hormone levels, reducing tension, and improving overall health. At least 30 minutes of moderate exercise per day is recommended.
- Sufficient sleep: Lack of sleep can wreak havoc on hormone levels and induce migraines. Seven to eight hours of sleep per night is the recommended minimum for women.
- Consultation: Women who suffer from migraines frequently should consult a healthcare professional. To regulate hormone levels and prevent migraines, seeing experts like the team at Melbourne Headache Solutions who can assess, diagnose and treat all the underlying causes of your migraine is essential to finding proper long germ relief.
Hormonal imbalances and migraines are significant health issues that impact a substantial proportion of women. As we observe International Women's Day, it is crucial to raise awareness of these issues and encourage women to take preventative measures. By addressing underlying hormonal issues via lifestyle modifications, women can reduce their migraine risk and improve their overall health.
How Hormonal Changes During Menstruation Affect Migraines in Women
Due to hormonal changes in their bodies, menstruation can be a time of discomfort and, in cases, agony for a number of women. Migraines are a prevalent symptom that many women experience during their period. In fact, up to sixty percent of women with migraines report that their headaches are provoked by their menstrual cycle.
First, it is essential to comprehend the function of hormones in the menstrual cycle. A delicate equilibrium of hormones, such as oestrogen and progesterone, regulates the menstrual cycle. Throughout this cycle, oestrogen levels rise and fall, reaching a peak just before ovulation and then dropping sharply just prior to menstruation. After ovulation, progesterone levels surge during the second half of the menstrual cycle. These hormonal variations can induce headaches. It is believed that the decrease in oestrogen levels just prior to menstruation is the primary cause of these migraines. When oestrogen levels decrease, the brain can undergo changes that result in migraines.

According to one hypothesis, the decrease in oestrogen levels alters the behavior of the brain's blood vessels. When oestrogen levels are high, the brain's blood vessels become more relaxed and less likely to constrict, which can lead to migraines. However, when oestrogen levels decrease, the blood vessels may become more sensitive to variations in blood flow, resulting in headaches.
A second hypothesis suggests that the decline in oestrogen affects the levels of other neurotransmitters, such as serotonin, in the brain. Serotonin helps control mood and pain awareness. A drop in serotonin levels brought on by a drop in oestrogen can induce a migraine.
Women can work with their healthcare provider to create a personalised treatment strategy. In order to control the levels of oestrogen and progesterone throughout the menstrual period, this may entail hormone therapy. To help manage migraines, women may also consider taking extra preventive steps like acupuncture, relaxation techniques, and exercise.
How Hormonal Changes During Menopause Affect Women's Migraines
Women are three times more prone to experience migraines than men, and they are three times more common. The onset of migraines can be significantly influenced by hormonal changes, and menopause is a key life stage that can significantly alter a woman's hormonal balance.
Menopause is a natural part of a woman's life that signifies the end of her fertile years. It is typically identified when a woman spans 12 months without having her period. The ovaries gradually stop producing eggs during this period, which causes oestrogen levels to drop. Hot flashes, mood swings, and sleep issues are just a few signs that arise from this hormonal change.

Migraines and menopause can interact in complex ways, and the nature of their connection is still unknown. Some studies indicate that migraines may become more frequent and severe during menopause, whereas others indicate that they may diminish. The following are some of the ways that hormonal fluctuations during menopause can influence migraines:
Hormone variations
Flashes of heat and sleep disturbances

Hot flashes are a prevalent menopausal symptom that can cause significant discomfort. They are sudden, intense heat sensations that can last anywhere from a few minutes to several hours. Flashes of heat can disrupt sleep and cause fatigue, which can cause migraines.
During menopause, sleep disturbances are common, and women may have difficulty falling asleep or staying asleep. Migraine risk is increased by sleep deprivation, and menopausal women who experience sleep disturbances may be more susceptible to migraines.
Stress
Migraines are frequently triggered by stress, and menopause can be a stressful time. It is a big change in a person's life that can cause both physical and mental changes. During menopause, women may feel anxious and depressed, which can raise stress, causing migraines.
Alternative therapies
Hormone replacement therapy (HRT) is a treatment that replaces the hormones depleted during menopause with oestrogen. Some women may benefit from HRT with a decrease in the frequency and severity of migraines, but it is not appropriate for all.
Additional migraine treatment options include triptans and anti-nausea medications. Changes to one's lifestyle, such as regular exercise, a healthy diet, and stress management techniques like mindfulness meditation, can aid in reducing the frequency and severity of migraines.
Women with a history of migraines may experience an increase in frequency and severity during perimenopause and menopause. Migraines during menopause may be treated with hormone replacement therapy, medication, and lifestyle modifications such as exercise and stress management. It is critical for women to discuss their symptoms and treatment options with their healthcare provider in order to determine the most appropriate approach for their individual needs.
Celebrating Women's Strength in Managing Hormonal Migraines
Women with hormonal migraines experience pain and disruption in their daily lives, and their strength and resilience in managing these headaches is worth celebrating.
Acknowledging the impact of hormonal migraines is the first step to celebrating women's strength in handling them. These migraines can cause severe pain, nausea, and fatigue, making daily tasks, work, and family life difficult.
Thanks to coping techniques, many women have been able to successfully manage their hormonal migraines, reducing their migraine incidence and severity by identifying triggers like stress or hormonal changes and adopting healthy lifestyle habits.

Medical therapy has helped many women manage hormonal migraines. Patients can work with doctors to create customised therapy plans. These plans may include painkillers, triptans, birth control drugs, or hormone replacement therapy.
Hormonal migraine sufferers are strong women who have learned to cope with chronic pain, sought medical care, and advocated for themselves and others. Celebrating women's strength in managing hormonal migraines can help reduce stigma and provide support for those who are suffering. We can better comprehend and treat hormonal migraines together.
Women who experience hormonal migraines demonstrate strength and resilience in coping with chronic pain. By seeking medical care and advocating for themselves and others, they inspire those who are struggling with this condition. Recognising and celebrating the strength of these women can help reduce stigma and provide support for those in need. Together, we can make progress against hormonal migraines by learning more and coming up with better ways to treat them.
How women can take action to stop menstrual migraines
To address menstrual migraines, it's important for women to understand that hormone imbalances may not be the only factor contributing to their migraines. Other factors such as liver issues, gut health problems, electrolyte imbalances, stress or anxiety, upper cervical nerve issues, and central nervous system sensitisation may also be involved. Therefore, it's essential to identify all the contributing factors in order to achieve the best results.
An approach may be to consider the following factors
CNS sensitisation and contributions from the cervical nerves and TMJ (jaw), so a thorough physical assessment is vital, even without neck pain being a prominent symptom.
Gut health: a healthy gut is crucial for balanced hormone levels. Addressing gut issues, such as gut dysbiosis, can help reduce oestrogen levels.
Support for detoxification: The liver plays a key role in oestrogen metabolism and detoxification. Supporting the liver through dietary changes and supplements can help reduce oestrogen dominance.
Reduce your exposure to toxins in the environment. Exposure to toxins like plastics and pesticides can throw off the balance of hormones.
Support healthy lifestyle habits. Regular exercise, techniques for reducing stress, and getting enough sleep can all help keep hormone levels, including oestrogen, in balance.
Nutritional support: Nutrients such as B vitamins, magnesium, and zinc are important for oestrogen metabolism. Ensuring adequate intake of these nutrients can help reduce oestrogen dominance.
At Melbourne Headache Solutions, we offer a comprehensive assessment procedure that considers all these factors to develop an individual treatment plan. This plan may include osteopathy, naturopathy, and acupuncture, among other approaches. Women can manage their menstrual migraines and improve their overall health and well-being by addressing all the underlying causes.
If you suffer from hormonal migraines, book a consultation with our experts today or you can visit us at melbourneheadachesolutions.com.au to learn more.
Your Questions Answered
What are progesterone headaches?
Progesterone headaches, common among women, occur due to changes in progesterone levels during the menstrual cycle, pregnancy, or menopause. These headaches are often severe and accompanied by symptoms like nausea, dizziness, and sensitivity to light and sound. Factors such as hormonal treatments or contraceptives can also contribute to these headaches. Understanding progesterone's role in migraine onset is crucial for effective management.
How can women manage progesterone headaches?
Women can manage progesterone headaches by identifying triggers, practicing stress reduction techniques, ensuring adequate sleep, and considering hormone treatments like birth control pills or hormone replacement therapy. These strategies aim to reduce the frequency and severity of headaches by addressing underlying hormonal imbalances. Consulting with a healthcare professional can help tailor a treatment plan to individual needs.
How do hormonal imbalances contribute to migraines in women?
Hormonal imbalances, including fluctuations in progesterone levels, can contribute to migraines in women by altering neurotransmitter levels, affecting blood vessel behaviour, and triggering inflammation or stress. These fluctuations disrupt the delicate balance of neurotransmitters like serotonin, influence blood vessel behaviour, and contribute to inflammation or stress, all of which can trigger migraines. Lifestyle modifications, stress management techniques, and hormone treatments may help mitigate migraine frequency and severity in women.
Follow us

